Rheumatic Diseases: Myths and Reality
What are rheumatic diseases?
 Rheumatic diseases are non-traumatic and non-surgical diseases of the musculoskeletal system and connective tissue diseases. It is the diseases of joints, tendons, ligaments, serum pockets, muscles, bones and spine. However, some rheumatic diseases, such as So-called autoimmune rheumatic diseases, are not limited to the musculoskeletal system, but they also affect various other organs or systems of the human body, such as Kidneys, skin, eyes, lungs, heart, arteries, veins, liver, brain, etc.
Rheumatic diseases are non-traumatic and non-surgical diseases of the musculoskeletal system and connective tissue diseases. It is the diseases of joints, tendons, ligaments, serum pockets, muscles, bones and spine. However, some rheumatic diseases, such as So-called autoimmune rheumatic diseases, are not limited to the musculoskeletal system, but they also affect various other organs or systems of the human body, such as Kidneys, skin, eyes, lungs, heart, arteries, veins, liver, brain, etc.
Are rheumatic diseases a problem for the elderly?
There is a widespread perception that "arthritic" affects older people and is therefore a predominant problem of the elderly. Indeed, some of these diseases, and even the most common ones, such as osteoarthritis and osteoporosis, challenge older people. In reality, however, no age is immune. The most serious rheumatic diseases, such as autoimmune rheumatic diseases (Rheumatoid arthritis - Systemic Erythema Lynx - Axial Spondyloarthritis - Systemic Scleroderma) not only affect younger and middle-aged people more often, but they are even presented to children.
What are rheumatic diseases?
Rheumatic diseases are many, about 200, and can be classified as:
1. Inflammatory rheumatic diseases
They are the prime subject of the rheumatologist, have autoimmune etiology and according to the target organ, include:
| Joint Damage (Arthritis) |
Rheumatoid arthritis,
Psoriatic arthritis,
Axial spondyloarthritis,
Juvenile idiopathic arthritis
|
| Muscle - skin infection | Polymyositis, Dermatomyositis |
| Salivary and exocrine gland damage | Sjogren's syndrome |
| Skin and internal organ damage |
Systemic lupus erythematosus,
Systemic scleroderma
|
| Vaginal Attacks (arteries and veins) |
Temporal arteritis,
Wegener's granulomatous antiphospholipid syndrome,
Adamantiadis- Behcet,
Arthritis Takayasu Kawasaki Disease
|
| Self-inflammatory diseases |
Mediterranean fever
Still's disease
|
| Crystallized arthritis |
Urinary arthritis
Pseudorubic arthritis
|
2. Degenerative type arthropathies
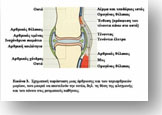
Osteoarthritis is the most common condition in this class and usually involves knees, hips, fingers and spine. Here, joint damage is not due to inflammation, but to the gradual destruction of articular cartilage (the "crisp" that covers the joints and allows for smooth movement), resulting in gradual joint deformity, osteophyte formation, pressure of adjacent Soft particles, etc. All this is accompanied by intense pain, deformities and joint dysfunction.
3. Diseases of extraarticular rheumatism
These conditions are related to periarticular soft molecules, such as muscles, tendons, with which the muscles adhere to the bones, the tendon sheaths, i.e. the tubular sheaths surrounding the tendons, and the serum sacs, I.e., small cysts containing a minimum amount of fluid and having as their main task the reduction of mechanical friction during muscle contraction and movement of the joints. Here, usually, pathological conditions are associated with over-stressing syndromes of the above tissues.
4. Metabolic bone diseases
This group includes osteoporosis, the most common of all, osteomalacia, Paget's disease and others. It should be noted that osteoporosis is the so-called "silent scourge" of our time, since, contrary to what is believed, it does not show symptoms until it is too late, when the first fracture, usually in the bones of the spine, Which, of course, besides intense pain, causes many other serious problems.
What are the symptoms of rheumatic diseases?
 The main characteristic symptoms of these conditions are:
The main characteristic symptoms of these conditions are:
How to diagnose rheumatism?
Often it is difficult, especially when joint involvement affects exacerbations and recessions or migraine (from one joint to the other) or when general and extraarticular symptoms predominate (see above). Although blood tests and imaging methods can help us a lot (and here it is worth noting the contribution of ultrasound in the imaging of joints and periarticular structures), nothing can substitute for the patient's clinical examination and a detailed history of The treating physician.
Is there a cure for rheumatic diseases?
Yes, today, thanks to advances in Rheumatology, there are great therapeutic options for treating rheumatic diseases. Rheumatology, the medical branch dealing with the study, research, diagnosis, prevention and treatment of rheumatic diseases, has made remarkable advances in the treatment of rheumatic diseases in recent years. And this has been made possible by our knowledge of the pathogenetic mechanisms of these diseases and the progress of biotechnology.
How Can We Treat Rheumatic Diseases?
The basic and necessary conditions for the treatment of rheumatic diseases are:
(Physiotherapists, occupational therapists, physiotherapists, psychologists, pediatricians, rheumatism associations, etc.)
|
The main goals of the treatment include:
|
Nearchus 18 | Chania
Telephone: 2821008940
Mobile: 6973356790



